Social media plays an ever-growing role in our lives on a daily basis. For many of us, we use social media every day, but understand very little of how it affects us.
Social media and drug use are closely related issues for teenagers. This is because substances and social media affect the brain in similar ways. They can both cause of release of high levels of dopamine which can lead to produce addictive behaviors.
Social media has a huge impact on how we interpret others, ourselves, and the world around us. For this article, we are going to focus on social media’s relationship with dopamine and the brain’s reward system.
What is Dopamine?
Dopamine is a neurotransmitter that can be released in the brain and is commonly associated with pleasure, satisfaction, enjoyment, and reward. This system is in place to reward us when we take positive healthy actions in order to ensure we keep taking those actions, and it’s also one of the primary ways that drug use affects the teen brain.
Drug Use and Social Media
The greater the reward, the greater the chance we become addicted. For most of human history, this risk has been mitigated by the fact that high-reward activities took hard work and long periods of time to achieve.
In today’s world of fast food, door dash, and internet food channels, we can access more food in an hour than our ancestors could access in a lifetime. The same is true for most other resources, and social media provides a convenient shortcut to receiving that reward.
Unearned Highs
As we discussed above, our brain’s reward system is in place to motivate us to take healthy actions. We have two routes to achieving these rewards;
- We can earn these highs through action and actually putting in the work required, or
- We can cheat the system and trick our brain into experiencing unearned highs.
For as long as the brain’s reward systems have been in place, humans have been finding ways to cheat the system, so to speak. Lying, stealing, cheating, fantasy, overconsumption, and manipulation are just a few of the tools we can use to try to cheat the system and experience rewards we did not earn.
The big tradeoff to our mental health becomes short-term pleasure for long-term pain (unearned highs), or short-term pain for long-term pleasure (earned highs).
Social media platforms play into this balance by offering an endless source of unearned highs, capable of tricking the brain into more dopamine “hits” than would normally be possible.
The Disadvantages
Through the internet and social media, people now have access to more information in an hour than what was available in a lifetime for previous generations.
There are many obvious advantages to this, but there are also some serious disadvantages. Social media plays a large part in a bigger cultural dilemma today which is dopamine saturation and immediate gratification by:
- Using likes, subscribes, comments, and many other measures of approval to feed our desire for attention and human connection. Each “like” gives us a little hit of dopamine, each subscriber gives us a little more.
- On top of that, we can live vicariously through others and get a taste of what it’s like to climb Mount Everest, be a millionaire, and get the love interest of our dreams all in a 15-minute window.
It’s no wonder so many people are glued to their phones. There are very few things in life that can provide that many quick fixes in short succession.
Dopamine: Social Media and Drug Use
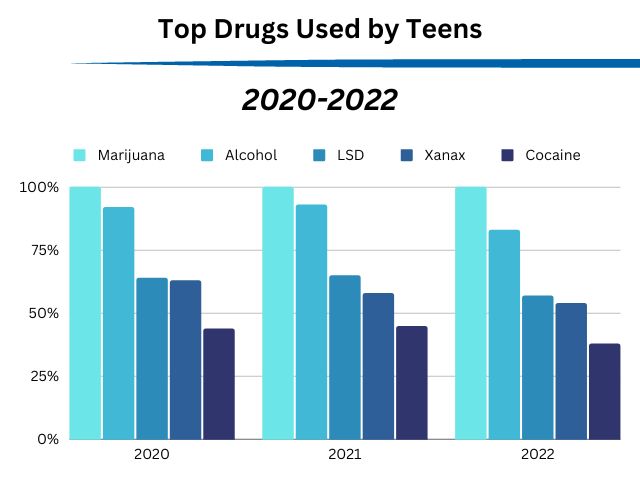
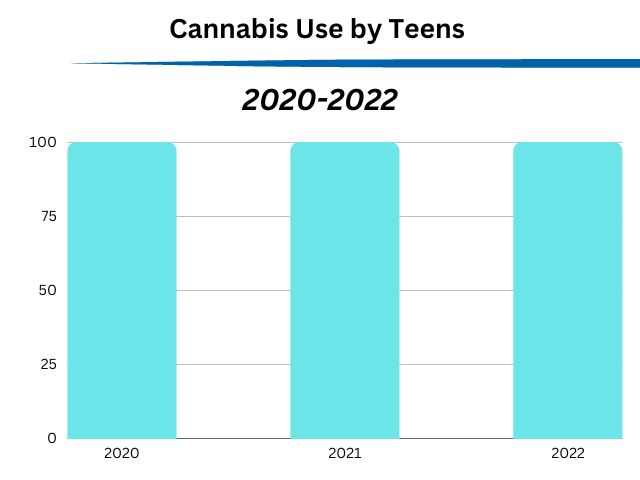
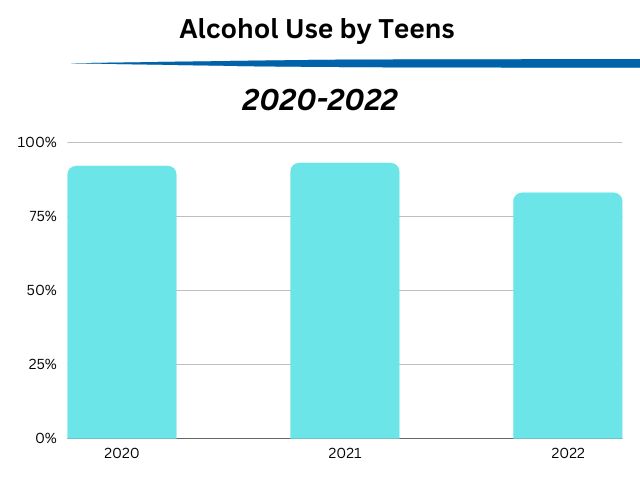
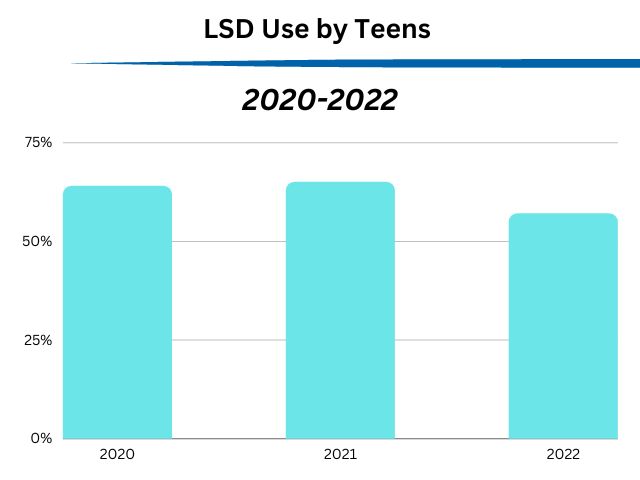
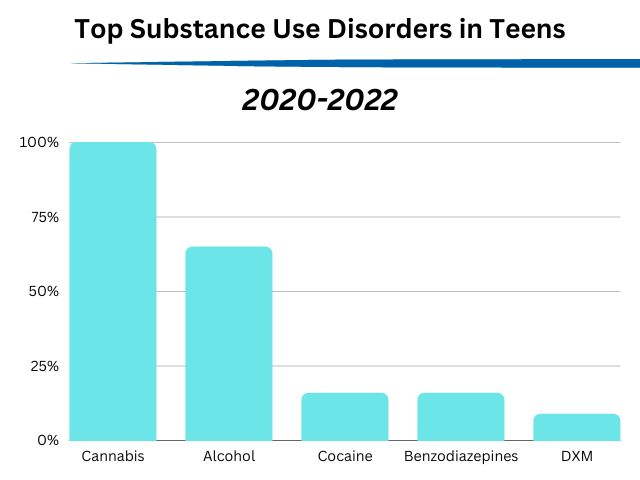
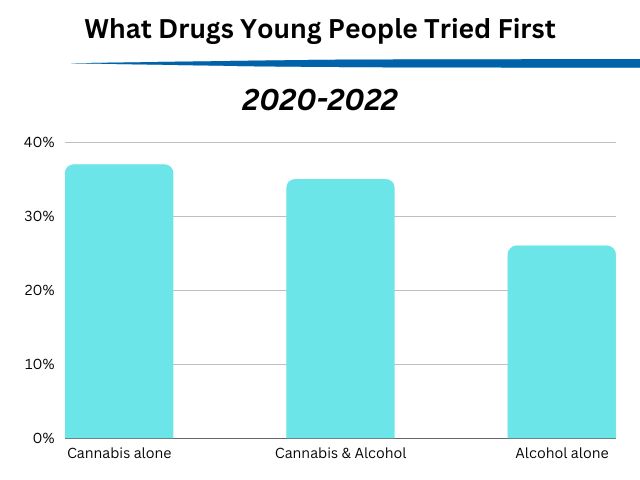
This is where the connection between drug use and social media comes into play. In a world where quick fixes drive our daily lives and drugs are more available than ever before, the quick fix of drugs isn’t a huge jump from all the other quick fixes we access daily. The most common drugs used by teens all operate the same way on the brain.
Drugs affect the brain in the same way social media does, tricking our brains into huge releases of dopamine. Obviously, drugs are much more detrimental, but the payout is also significantly higher.
Effect of Social Media on Recovery
The connection that we consistently see at The Pathway Program between social media and substance use disorders is that both feed into the negative cycle of addiction in the brain, giving us quick fixes and demanding more and more as time goes on.
It is very common to see a person in recovery completely addicted to popular social media. Many of the teens and young adults we work with, come into addiction treatment with a drug abuse problem; along with an unhealthy obsession with social media.
In recovery, the young people who continue to feed into social media addiction are rarely capable of long-term recovery. The addictive cycle demands more reward, and always leads to relapse, if not broken.
What’s the Solution?
So, how does social media influence drug use? They both involve seeking unearned highs, which is a behavior that only results in further addictive behavior and mental health problems.
The solution for both issues involves finding ways to achieve self-worth, approval, positive relationships with friends and families, and positive experiences through earned highs, and to limit the negative behavior patterns of addiction and rush-seeking behavior.